Compliance of primary and secondary care public hospitals with standard practices for reprocessing and steam sterilization of reusable medical devices in Nepal: findings from nation-wide multicenter clustered audits | BMC Health Services Research

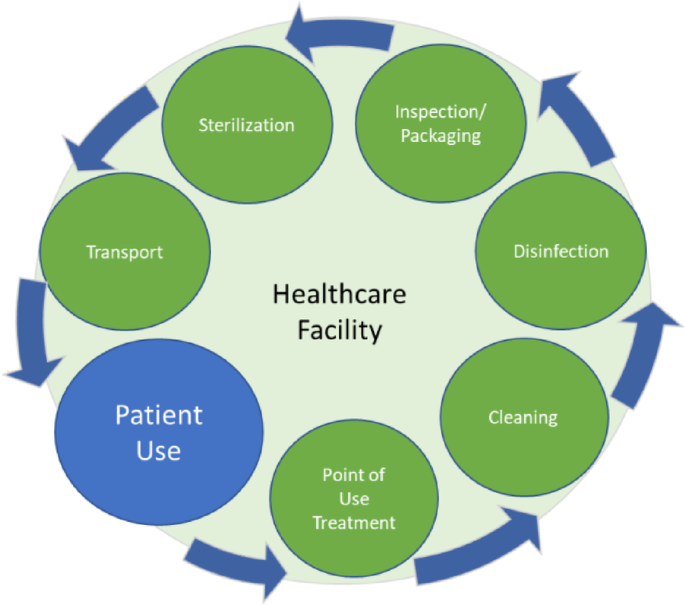
The mean percentage compliance with standard practices for the reprocessing of reusable medical devices achieved by all the primary and secondary care public hospitals in Nepal was only 25.9% (95% CI 21.0–30.8%). There is no standard cut-off value for percentage compliance with these practices. A high value of the percentage compliance indicates that most of the standard practices for medical device reprocessing are followed by the hospitals. Compliance with the standard practices helps hospitals ensure safety, reliability and quality of medical device reprocessing [48]. Therefore, it is important for the hospitals to comply with the standard practices for ensuring the required SAL of medical devices. In this sense, the compliance of the primary and secondary care hospitals in Nepal with the standard reprocessing practices is poor. The mean percentage compliances for each process of the reprocessing cycle were less than 50%. These findings are in line with the high proportion of steam sterilization failures (reported elsewhere) in these hospitals [18]. One factor that may have led to overestimation of the mean percentage compliance is the presence of the researcher (auditor) during the reprocessing activities. The staff involved in medical device reprocessing may have become more attentive due to the presence of the researcher and hence, they could have performed the reprocessing activities more carefully on the days when the researcher was present than on ‘normal’ days.
The reasons for the poor compliances are not clearly understood. We previously reported that more than 50% of these hospitals did not have dedicated space for reprocessing of medical devices, and only one of the thirteen hospitals had sterilization procedure manuals or flow charts. Similarly, only one hospital had spare parts for the sterilization equipment and none of the hospitals had equipment maintenance records. Moreover, only 1 to 3 staff were assigned for medical device reprocessing in these hospitals [18]. In this study, we found that, for more than 97% of the reprocessing cycles crucial processes, such as cleaning and autoclaving, were carried out by support staff (i.e. office assistants). The level of education of support staff is very poor i.e. either completion of some years in school or no formal education. These findings indicate that there could be several reasons for poor compliance related to management and support processes including infrastructure, human resources, equipment, guiding documents, steering, performance monitoring and documentation. As the higher-level hospitals, compared with the lower-level hospitals, should have better management and support processes, the higher average percentage compliance in these hospitals is to be expected.
About 92% of the reprocessing cycles had sterilization loads with porous items such as linen and more than 46% of the cycles had loads including items with channels or tubing, such as dental hand pieces and laparoscopic sheaths. Air in all cavities and spaces within such medical devices needs to be replaced with steam for proper sterilization. Air removal is more difficult with such items and active air removal is usually recommended for ensuring the attainment of sterilizing conditions [4, 40]. None of the steam sterilization processes used by primary and secondary care hospitals in Nepal had an active air removal process such as pre-vacuuming [18]. No specific sterilization processes were designated for medical devices having specific designs, and devices with different designs were included in a single load. Such practice in the absence of an active air removal process is detrimental to the achievement of efficient sterilizing conditions within the load.
Safe transportation of used medical devices is important to minimize microbial contamination of the surrounding environment, and also to minimize the risk of device-associated infection among healthcare workers and patients. A rigid, durable, leak-proof container with a tight-fitting lid is recommended for transportation of used medical devices to the decontamination area [47]. However, for all of the reprocessing cycles in the hospitals in Nepal, used medical devices were either transported in an inappropriate container or transported without using a container. Such an inappropriate handling practice may be putting healthcare workers and patients at risk of injuries and/or exposure to microorganisms.
Cleaning was done in a designated dirty area for only 38.1% of the reprocessing cycles. Cleaning of medical devices in areas where other activities such as hand washing, dish washing, food preparation and drinking are performed, poses a risk of contamination of other areas and thus increases the risk of transmission of microorganisms to healthcare workers and patients. The risk of transmission of microorganisms was further amplified by the practice of cleaning medical devices without submerging them in water. Washing medical devices without submerging them in water may create splashes and aerosols, which might not only transmit microorganisms, but also can also increase inhalation of disinfectant by the cleaners and increase contact of mucous membranes (e.g. mucous membranes of eyes and mouth) with the disinfectant.
The risk of infection among cleaning staff was further increased by very poor compliance with the recommended use of PPE. Though gloves were used during cleaning for most of the reprocessing cycles, use of eye protection, protective clothing and facemasks during the cleaning process was rare. A study conducted in one of the largest hospitals in Nepal found that 20.9% of “non-professional staff”, 19.2% of nurses, 5.6% of laboratory workers and 3.1% of doctors had evidence of past or present HBV infection [49]. The authors of the study claimed that higher occurrence of HBV among “non-professional staff” and nurses was because of their involvement in the cleaning of medical devices without proper measures to protect themselves and the lack of adequate HBV vaccination. The findings of our study support the claim made by these authors.
Medical devices were cleaned manually for all of the reprocessing cycles in all of the hospitals. Automated washers are commonly used in many countries for cleaning of reusable medical devices, but studies have found that both manual and automated cleaning processes are effective in reducing the microbial load on medical devices if executed properly [50, 51]. Manual cleaning processes are more prone to human error compared to automated processes. Ofstead et al. (2010) found adherence to endoscope reprocessing guidelines for 1.4% of endoscopes reprocessed manually, and for 75.4% of endoscopes reprocessed with an automated endoscope cleaner and reprocessor [52]. We found variations in manual cleaning processes in the hospitals of Nepal as well, the process varying from single-step cleaning using plain water to three-step cleaning using disinfectant, detergent/soap and plain water.
For about 82% of the reprocessing cycles, the cleaning process included pre-soaking of medical devices in a hypochlorite solution. In the absence of proper and consistent use of PPEs, the practice of pre-soaking might have provided some protection to the staff handling used medical devices, however, this practice could have deterred staff from the proper and consistent use of PPEs. Recent guidelines recommend not pre-soaking medical devices in a disinfectant before cleaning [4]. The reasons behind this recommendation are corrosion of the devices due to disinfectants, inactivation of disinfectant by blood and body fluids, risks to health-care workers while transporting the soaked items and possible contribution to the development of antimicrobial resistance to the disinfectants [4]. However, in the case of Nepal, if pre-soaking in hypochlorite solution were to be avoided, the practices of cleaning medical devices immediately after the procedure (usually within 1 h) will become crucial for effective cleaning of medical devices and the prevention of formation of biofilms on medical devices [53].
Cleaning of medical devices is a critical step for reprocessing of medical devices, as it significantly reduces bioburden on the surfaces of medical devices [51]. However, this is not as simple as it may appear. Staff responsible for cleaning of medical devices need to have a clear understanding of microorganisms and the importance of cleaning in medical device reprocessing. Seavey (2009) highlights the need for educating staff involved in reprocessing activities at least in the areas of basic medical terminology, human anatomy and physiology, microbiology, infection prevention and control, regulations and standards, surgical instruments, and all processes of reprocessing cycles [54]. In an ideal context, monitoring of cleaning processes using a validated scientific monitoring technique is recommended for ensuring adequate cleaning of medical devices [55]. However, support staff (office assistants) with very poor education level were involved in the cleaning of medical devices for almost all (98.4%) of the reprocessing cycles in the primary and secondary care hospitals. A required level of cleaning of medical devices is unlikely to be achieved without having properly trained and educated staff undertaking the reprocessing of medical devices.
For all the reprocessing cycles sterilizing wrapped medical devices, linens were used as the wrapping material. Previous studies have demonstrated the effectiveness of linens in maintaining sterility of wrapped medical packages [56, 57]. Currently, there are various options available for packaging of medical devices including rigid containers, peel pouches (plastic and/or paper), and woven and nonwoven wrapping materials. Based on cost-effectiveness and suitability, such options also need to be explored and used by hospitals for continuous improvement in medical device reprocessing.
Orientation and loading of channeled medical devices inside each medical device package and that of the packages in each sterilization load could not be recorded in this study. However, it is important to ensure that the packages are loaded ensuring adequate circulation of steam inside each of the packages and channeled and hollow devices are positioned inside the packages in such a way that accumulation of condensate inside such devices is avoided [58].
Most of the standard practices for steam sterilization (autoclaving) were not followed for most of the reprocessing cycles. No chemical or biological indicators were used to monitor the effectiveness of sterilization, except for the use of indicator tape for fewer than 50% of the reprocessing cycles. Indeed, autoclave tapes do not measure the effectiveness of autoclave cycles; they only indicate an exposure of a package to a heat/pressure-based sterilization process [59]. Additionally, none of the sterilization cycles had variable parameters (time, temperature and pressure) recorded. Though all the autoclave cycles were manually operated, timers were used to monitor sterilization holding periods for only a small proportion (i.e. 6.4%) of autoclave cycles. This showed that medical devices were being reused without having concrete evidence of their sterility. Information such as load number, operator, and sterilization date and time were also not recorded. In the case of an incident (such as surgical site infection) likely to be associated with reusable medical devices, it would be difficult to trace the sterilization load, person sterilizing the load, or the date and time of sterilization. This indicated that it was unlikely that the possible source of infection would be identified, thus preventing correction of faulty practices.
For the majority of the reprocessing cycles, sterilized packages were wet or contained moisture. The wet sterilized packages could have been associated with one or more factors including quality of packaging material, packaging technique, loading technique, sterilization process, sterilizer, steam quality and storage area [60]. Moisture can facilitate the entrance of microorganisms to the sterilized packages. In general, wet sterilized packages are considered as contaminated, and should be re-sterilized before use, and wet sterilized porous loads such as textiles can be even more problematic [61]. Some studies conducted in Nepal have shown that different microorganisms including Staphylococcus aureus, Micrococcus spp., coagulase-negative staphylococci, Bacillus spp., Pseudomonas spp., Acinetobacter spp. and yeasts exist in hospital indoor environments [62, 63]. In these settings where sterile storage conditions are not controlled, the chances of contamination of wet packages with microorganisms could be high. None of the wet sterilized packages were subjected to re-sterilization in the hospitals in Nepal. There is a need for a thorough assessment to establish the causes of wet sterilized packages to formulate recommendations for solving the problem.
The absence of routine inspection of packages after sterilization for integrity was observed in all of the hospitals. The absence of inspection of sterilized packages could also be linked with the practice of not re-sterilizing wet sterilized packages discussed above. There were gaps in transportation and storage of sterilized packages which did not favor long-term sterility of medical devices, which was further compromised by wetness of sterilized packages.
The findings of this study may not be able to be generalized to tertiary care public hospitals (i.e. central hospitals) and private hospitals in Nepal as these hospitals were not included in the study. The study also did not cover smaller public and private healthcare facilities such as primary health centres, health posts, private outpatient clinics and private dental clinics. However, the findings of this study can be useful for the improvement of medical device reprocessing in these healthcare facilities as well.
link